Mentorship Program Information
Information on my new mentor program
When you're finishing your apprenticeship or schooling and figuring out how to start a practice, trying to figure out if you're truly ready or if you need more, it feels isolating. Every choice feels like you're reinventing the wheel.
If you're choosing not to license or take the NARM, there is another layer of insecurity and lack of continuity from preceptors and schools to make sure the midwives being trained are supported as they go on their own. You don't have a piece of paper saying you're ready, you only have your gut, possibly the school or preceptor, and hope.
Even if you've been the primary midwife for a while, those first clients you get under your own name can make or break your journey.
This program is to support you, in whatever you need. I started my practice on my own, without support from anyone, in 2019. And I made so many mistakes. I had my classmates to reach out to, I had a couple elder midwives, but I was truly on my own making sure this worked. And in 2021 I almost burned out completely.
I don't want you to go through that. I want you to have the business you desire, the clients you crave, all while knowing someone has your back. You shouldn't be in this alone and you should have someone in your corner.
This program is not permanent. I do not want anyone to feel like they have to continue needing an intense level of support to continue being a midwife. I want this to be a stepping stone, a way for you to find more confidence, so at the end of six months to a year, you are ready to fly. At the end, I am not pushing you out, but you will move on to a different level of support from me, and the community I hope to build.
In this program:
You will have access to me (within limits, like I will not be texting back at 3am for non-emergencies, just like my own clients) through text and video. I have Marco Polo, Voxer, Messenger, DM on IG, WhatsApp, GroupMe, and Telegram. All are available to you, whichever is easiest, though the group chats will be on GroupMe and Marco Polo for ease.
Access to me can look different for everyone. The people that I have helped before, it has been questions about different topics related to their clients and themselves, such as:
Blood work walkthrough
Symptoms clients are dealing with, ways to narrow it down, and possible treatments
Information they've read and have questions about
Talking through videos and posts they've found online to see what could be done differently or what it all means
Discussing their practice, including forms, resumes, information
Helping them feel confident in the skills they possess, while making a plan for things they are worried about
Narrowing down who they want to help and why
There really are no limits to what you can ask or receive.
I am only signing up five people to start, to make sure each person receives the help they want and need and I am also not overtaxed. I also only take on 5-7 clients of my own every year for this reason, making me accessible to everyone that needs me, including my family.
Twice a month, you also have the option to schedule an hour long live mentor call with me, should you choose. This will be used to go more in depth on anything you need and create plans going forward. Sometimes it could simply be a way to vent about something, while other times we discuss everything you've been working on or what you've been doing.
In addition to the mentor calls, you can also debrief with me after every birth, if you want it. Even the good births! Celebrating the triumphs is just as important as walking through the hard situations together.
The group chats are a place where everyone signed up can talk to each other, but no more than 5 people in the group plus me to keep it small and less overwhelming. It's also a way to crowdsource questions and get support from more than just me. We all need a community and sometimes we just need to build that ourselves.
Twice a month I will be leading live video calls:
One on business with topics like
Forms
Practice protocols and routines
Charting
Websites and Social Media
Peer Review (every 2 months)
Ideal Clients
One on education topics like
Blood work
Shoulder Dystocia
Birth Video viewing
Newly released research
VBAC
NRP
I want them to be an open discussion as well, not just me lecturing, so figuring out when everyone can attend will be important. Things happen and not everyone can be there all the time, but maximizing it will be really helpful for growth and the need for community building. They will be recorded and posted so you can watch whenever you wish.
You will also get access to all of the forms, flyers, and books I create, along with all my bookmarks. I have a lot of resources and making sure everyone has access to all of it is important. You may want to create your own or just use mine, either way is up to you. Most of the things I create are available to buy on my website, but through this program, it's all included for free.
You are also automatically added to my discord server through the Patreon, but you do not have to use it. I'm hoping to build it up more this year so we have a great group of birthworkers that can all support each other, but that's not the main goal of this program.
We aren't supposed to be Midwives alone. We are supposed to have support that looks like all of this so we can find our own place in the world. Most midwives don't make it to five years, and I want everyone to have the support to go as long as they wish, not ended for burnout or other reasons.
The course is $150 a month or $744 if paid 6 months in full, plus $1 a month to the site. I am using Patreon as the platform for now, and if you pay in full you need to subscribe for $1 a month to have access to everything, which is why I've removed the $6 from the total fee paid to me.
Sign up below! If the program is full, please join the waitlist!
How Did I Get Here - Part 3
When you look back at certain events, especially as time passes, different things stand out to you.
I wonder if part of it is your brain trying to make sense of what happened, to find some meaning or depth. But sometimes it just feels like a scratched record skipping and playing the same three notes over and over until you want to scream in frustration and pain.
You can see the rest of the series here
————————————————————————————————
When you look back at certain events, especially as time passes, different things stand out to you.
I wonder if part of it is your brain trying to make sense of what happened, to find some meaning or depth. But sometimes it just feels like a scratched record skipping and playing the same three notes over and over until you want to scream in frustration and pain.
I hear the beeping of the monitors and feel my legs squeezing. The room is much smaller than the one earlier, and the window is on the opposite side. My arm hurts where the IV is. And my abdomen burns.
And then the guilt follows.
Last night I thought it would be so neat if my baby was born today. The consequences didn't matter, what a neat birthday it would be. My partner comes in and tells me what he knows - our baby is in the nursery on oxygen. He doesn't know anything else.
A nurse brings a polaroid of my baby, because I can't get out of bed to go see her. Why? I still don't know. It's probably nearing 4pm, but time means nothing to me because nothing makes sense. My parents are there, they saw her through the window of the nursery. They bring some gifts for me, for the baby. That I still haven't seen.
Everyone keeps calling to say congratulations. How do you handle that when you aren't even sure that you had a baby? Maybe it was just a bad dream and I'm going to wake up soon to go to the hospital.
Finally, at 9pm, almost 8 hours after she was born, the nurse comes in and says she is there to take me to see her. It takes about a half hour to get everything set up and wheel me down.
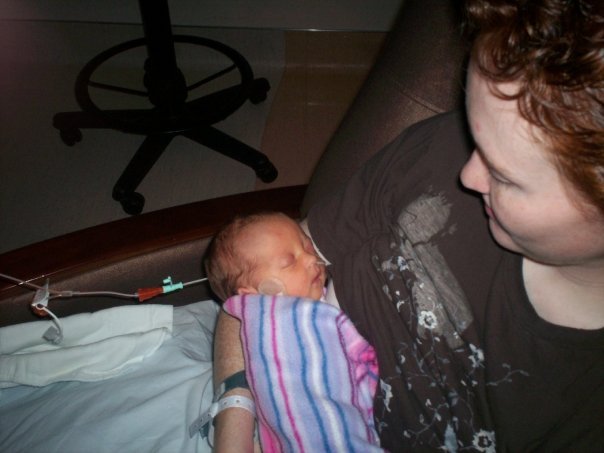
She's on oxygen. With an IV. She has a green pacifier, naked except for a diaper. She looks bruised and has hair on so much of her body. She has so much dark hair and is so tiny.
She doesn't feel like mine. How could she? She exists outside of me now and I hadn't seen any of it. That will take months to heal, made worse when she's transferred.
I am not allowed to hold her. She is struggling with oxygen and they are worried about her, so I hold her hand. What kind of mother can't hold her own baby. We only stay for a half hour.
I sleep fitfully. They brought me a pump, so I was doing that every two hours around the clock. The nurses joke that I'm doing so well because I'm getting 1 ounce every time only hours after having my baby. I don't know any different. They place the milk in orange snap top containers like what camera film was in. They don't tell me to not overfill it. Almost all of it had to be thrown out when we got to the next hospital because they weren't sealed and the milk wasn't safe. I had about 30 ounces when we went two days later, and they could keep maybe 10 of them.
I slept and ate and pumped and took meds and let them push my belly and showered the next day and got the catheter out and hoped I could hold my baby eventually. She was 24 hours old when I finally did, with the help of nurses because she was sent next door to the higher level nursery when her oxygen level needs kept increasing.
I held her. She was so small. Five pounds. I didn't know what questions to ask or how to feel, just hoped it would make sense eventually.
My partner held her, all the while my mom was with us taking pictures. We stayed for an hour or so and then had to leave. My in-laws were there, meeting her through the window. The first grandchild for both sides. What a special time, right?
Time passed, she never left the nursery, and we would get updates often with how she was. She was born Wednesday, by Friday they were talking about discharging me on Saturday, but she probably wouldn't be. I was able to walk to the nursery then and see her, but I still had to have a nurse escort me and stay with me, and it felt even more like I had no idea how to take care of this baby without someone making sure I wasn't doing something wrong. We didn't get to hold her again before Saturday, her oxygen needs kept increasing and they told us she might need to be lifeflighted to another hospital because she was almost at the limit they were allowed to give.
Nod. Smile. Hold her hand. Pump. Meds.
Friday afternoon the pediatrician came in to tell us she was being sent an hour away. The team was called and had to get her set up so they could go because she needed more help.
Have you ever had those experiences when everything is in slow motion? You hear words but they don't really click and you wonder what is happening because it doesn't really make any sense? I knew she was being sent away. I knew I was still a patient at this hospital and couldn't leave. I knew my partner was not ok. So, I put everything I felt aside and prepared to go.
A wonderful nurse called the hospital and asked if we could have a place to stay while she was in the NICU, and they had a room set up for us in the PICU. It was evening and too late to set up at the Jubilee home, and they weren't sure they would even take me since they were hoping it would be a short NICU stay. I called family and let them know. I packed everything. I went to see her and had to leave because they had to get blood from her and I couldn't handle them poking her over and over.
She hadn't had any food up to this point. Just an IV. Getting her to bleed was an entire expedition, the team later told me. She was hydrated but it just wasn't enough and she had so many sticks that her heels were raw. It hurt to see it, and so I didn't.
They put her in a helicopter and left. We followed, after going to the store and buying a pump, and an hour later we were at the hospital. They got there long before we did, and as soon as we pushed the button for the NICU, a nurse was there to meet us and explain how we had to come in and wash our hands and prepare to see her. When the new hospital was built, it was so weird to go in and see the NICU wasn't behind a locked door and you only needed hand sanitizer to go in. We had a full sink, with timers on how long to was our hands. And this had to happen every time we entered.
We go into her room, and she already looks amazing. She's less red, she's breathing easier. The neonatologist, who would become one of my favorite people, told me everything that was going on. She didn't need to be intubated or put on CPAP, just the lower elevation may do the trick to help her breathe. He explained different things they had planned if anything needed to be done, and they had already got a feeding tube in and with the milk I brought, they would start to feed her to prepare for me to nurse her.
It was surreal. This high level facility, where things were locked down and we had to wash like surgeons was treating me more human than I had felt in the last two weeks. They helped us get set up in our room, brought a hospital grade pump for me to use, containers for my milk, and cleared an entire shelf of the fridge for me. I was included and seen. This was not what I expected.
Saturday she increased her food intake each meal, getting ready for me to start nursing her on Sunday. Her oxygen needs were going down, she looked great. She had lost a lot of weight, over a pound, but they were excited at how much she was improving.
We went to eat with family, shopped around town, the last Harry Potter book came out and my mom bought it for me for something to do. I read it before we came home the next Wednesday. We hung out with our daughter for a couple hours every day, but I was young and inexperienced and had no idea what to do, and it was easier to let the nurses do it.
Sunday we started nursing. It was so weird. Why did no one tell me it was so weird?! But she was doing ok, though not eating as long as they wanted her to. She still had the feeding tube, even though now I was pumping 4 or 5 ounces of milk every two hours, so that definitely wasn't an issue. But it was just because she was small and tired and they wanted to make sure that she was still being fed. The lactation consultant came in and was so rough with me, and I still had no idea what I was doing when she left.
And then a nurse came in. She sat with me while I felt overwhelmed trying to get my baby to eat, told me I was doing great, that she was doing great. She answered my questions, but mostly she just made sure I was okay.
We take that for granted sometimes, I think. I didn't really need her, but her presence made all the difference to me. I still didn't know what I was doing, but I felt more like I could handle it after she left. I don't remember her name, and that is one thing I regret. She made such a difference to me and what happened, and I am forever grateful.
Monday brought jaundice. I knew I had it as a baby, but they were growing increasingly worried. Her levels were 15 and then 19 and then 21. They told me if they got to 22, she would get a transfusion. She lived in the bili bed on Monday and nursing was hard because she was so tired. But, she was finally pooping, and was still eating every couple hours, which was huge. Monday night I got to her room to nurse and they were so happy to tell me her level was down to 19 and things looked like they were getting better. She still needed the lights, but it was less dire, and we were doing it.
I nursed every 2 to 3 hours, and Tuesday brought hilarity when she ripped out the feeding tube herself. I should have known then that this baby was going to be a spitfire and do things exactly how she wanted them. They thought about putting the tube back but decided to see if nursing would be enough and left us to it.
We had to watch these videos before she was able to leave and they wanted us prepared, so we watched one on abuse and one on feeding and I think one on carseats, but I don't remember much anymore. Tuesday was over so quickly and it was surreal that she was almost a week old.
Wednesday my partner decided to drive home and go to work, and I swear, he had barely been there for 20 minutes when the hospital told me she was going home today. She had been off oxygen for about 30 hours and was doing so well, her jaundice levels were down to 12, and it was just unreal that this was our life.
She had to have a carseat test and her hearing screen and they had to explain everything to me. She was being sent home with oxygen because we lived 3000 feet higher and sometimes babies just have a hard time with the elevation. We had an appointment to see her pediatrician on Friday and he would tell us what to do.
By 1pm, we were out the door.
With a baby.
How in the world did you take care of a newborn???
Crash course, here we come.
How Did I Get Here - Part 2
“Walking into the hospital my gut was *screaming*. This isn't right this isn't right this isn't right. Over and over and over. It's like you're watching it happen to you in slow motion but there is nothing you can do to change the outcome.”
Part 2 of my new series about what brought me to midwifery and birthwork.
This part is the ECV and cesarean. It isn’t pretty. I’ve written this story so many times over the last 16 years, and this feels the truest. I continue to give myself grace, but I also see now how dehumanized I was through that entire day.
To read the other parts, head HERE
—————————————————————————————————
Do you ever have those moments where you know your life is going to change, and your gut is telling you to go back to bed because it's not a great change but something that will irrevocably hurt?
Waking up on the morning of my ECV was like that. We had to be at the hospital at 5am, and I didn't sleep well the night before, mostly nerves and excitement that I could possibly meet my baby that day. I didn't think I would, but it's that tiny part of your brain that thinks about what could happen? And I foolishly thought that even if we met our baby that day that everything would be great.
Walking into the hospital my gut was *screaming*. This isn't right this isn't right this isn't right. Over and over and over. It's like you're watching it happen to you in slow motion but there is nothing you can do to change the outcome.
I walk up to the nurse's station, and they have NO IDEA I'm supposed to be there. There are no orders, no forms, absolutely nothing saying that I am having an ECV at 7am. I'm barely 20 years old, I've done everything I'm told this entire pregnancy, and now they're saying I'm wrong and shouldn't be there. I stare, bewildered.
A nurse takes pity on me and takes me to a room and says they will call the doctor and figure it out. She hands me a gown, tells me I just need to take my bottoms off but can keep my shirt on (this is an issue later, just like everything else that day).
And we wait.
And wait.
And wait.
Finally, at 6:30, the nurse comes in and says that they got it all figured out and the anaesthesiologist is on the way to give me the epidural, and they just need to get my IV set up so everything can start.
It's like a giant rush at this point. No one was prepared but now they know they're on a clock and if they aren't ready when the doctor gets there, it's his time everyone is wasting, and somehow it's my fault for coming in without orders (even though there were, they just lost them along the way).
The epidural is placed, which I would never ever like to live through again, meds are placed, I start feeling a bit loopy, and finally my midwife and the doctor come in, all smiles. At 8:30am. What even is time anyway?
Ultrasound.
More meds.
Ultrasound.
So much talking.
The bed flattened and I'm lying on my back with my head a lower than my body to pull her out of my pelvis.
Pushing.
It's hard to breath.
More pushing.
Swearing.
Hands leave my belly.
Ultrasound.
"We got her halfway and then lost our hold and she went right back, we have to try again."
Pushing.
Pulling.
My whole body is jerking on the bed.
It's hard to breathe.
Pushing pushing pushing.
Finally release.
Ultrasound.
"We got her head down, everything looks great, good job! We need to keep you on the monitors to make sure baby is okay, just rest while the epidural wears off."
It worked. My baby is head down. The epidural needs to wear off and I can go home. I breathe a sigh of relief, knowing that everything is going to be okay.
I try to sleep a bit, but an hour later I wake up with my legs spasming on the bed but I couldn't feel them. I then proceed to have a massive panic attack, Blake can't calm me down, yells for the nurse. She comes in and helps me breathe and relax, but the twitching won't stop and I still can't feel my legs and what is wrong and why is this happening and when can I go home and and and and and….
They never told me a side effect of the meds was anxiety attacks.
Just chalk that up on the board of things I was never told, which gets longer by the second.
Slowly the feeling comes back to my legs. It's around 11am at this point.
And then my room is filled with nurses. Her heart isn't looking as good as they want, and oh crap, there is a pool of fluid on the pads under me.
During pregnancy, I remember being told over and over that if you have contractions 5 minutes apart, lasting one minute, for one hour, to go in to the hospital because that's labor. I was admitted twice in pregnancy for this - once when I was so dehydrated from puking nonstop for 24 hours, and once at 35 weeks. They laughed at me because the vaginal check showed nothing, even though the monitor showed contractions. I was patted on the head, told it's "just braxton hicks" and to come back when it's serious.
With your first baby, how are you supposed to know it's serious? How are you supposed to know that the 5-1-1 rule is bull when your uterus contracts every second of every day no matter what you do?
The list of things just gets longer.
My panic subsided with the adrenaline now filling my room, but I have no idea what could be wrong. The doctor comes in and tells me the baby isn't handling things as well as we would want, and my water might have broken, so they need to do tests for that and monitor me more closely to see if the baby perks up or if I'm in labor.
Um. Ok? This wasn't part of my plan. I was supposed to be going home.
Vaginal check. Dilated to a 1, same as 35 weeks.
Amniotic swab. Negative. What could this liquid be if not amniotic fluid?
Oh. They never placed a catheter. I had peed all over myself. Just great. Exactly what I want to hear when someone is sitting basically in my vagina.
Looking back, the most dehumanizing part of this is how they would talk about me like I wasn't there. I'm lying on the bed, still too numb to walk but getting feeling back, and they are talking to each other over me like they're talking about the weather outside. Like I am not even there to hear them.
At that moment, I knew my baby wasn't acting right on the monitor, I had in fact peed myself instead of my water breaking, and I wasn't in labor. They kept asking each other if they should put a catheter in, if they needed to walk me to the bathroom, if they needed to call the doctor, if they should flip me or sit me up, or or or or.
Never once did anyone look at me, explain what was going on, and ask if I was okay. Not once.
It's noon or 12:30, and baby is still having decels and I am now contracting regularly. But no dilation, after another incredibly rough vaginal exam that this time I can feel because I am no longer numb.
Still no words directly to me. Just at me and around me.
1pm, the doctor comes in. Finally, eye contact.
"Your baby isn't handling the version well, it's time to do a cesarean. Are you numb still?"
"No."
::turns to nurse and talks to her, never looking at me again::
I'm shaved.
Anaesthesiologist enters the room again, adds more medication to the catheter because they never removed it.
Notices I'm wearing a shirt.
Chaos ensues.
It was just a T-Shirt, but I have an IV, the epidural, and monitors all over my body. Taking the t-shirt off was a nightmare. And they had to do it quickly because the OR was set up and waiting.
The nurses ended up lifting and pulling me like I was a rag doll as they got the shirt off around everything, and then put my gown back on as if I had any shred of modesty or respect for myself left. None of that existed anymore, I didn't feel like a human at that point anyway. I was invisible.
The meds aren't working and I can still feel everything. Every couple minutes the doctor uses a pin or something to poke my legs to check if I'm numb. I'm not. Over and over.
He tells me that the dose he gave me is the same as earlier, but it isn't working. So he gives more. And more. And more. By the time I start to go numb, he tells my husband he's given me three times the normal dose, and he has to monitor me really closely.
Not to me, my husband.
Invisible. Still. I'm a body housing a baby that needs to come out. Nothing more.
They wheel me out of the room, Blake enters the OR after they get me set up, no one knows if I'm numb, but they start to cut and the anaesthesiologist says "oh good. She's numb, or else she would not be still right now."
Pulling.
Burning.
Pushing.
Talk about what they're doing after this.
Pulling.
Then the room is silent.
"We have a daughter."
No crying. No sounds.
I watch Blake's face as he watches them take her to the side of the room.
My arms are going numb from being strapped to my sides.
No sounds.
Finally, two small cries, then silence again.
They ask Blake if he wants to go with them to take the baby to the nursery, she's having a hard time breathing. He goes, and I am knocked out.
I wake in recovery, foggy and unaware. The nurse says I'm doing well, the baby needed extra care, and I go to sleep again.
It's a couple hours later when I wake up in my room, completely alone.
How Did I Get Here - Part 1
“Because if I hadn't asked questions the entire pregnancy, why start now?“
Every Monday, I will post a new part to my own personal birth history. This will not be happy most times, but over the years I’ve given myself a lot more grace and love, and I hope the story reflects that. I don’t know right now how many parts this will have, but it’s going to cover almost a decade of how I truly got to where I am. I’m not going to gloss over hard things, and be aware there is talk of cesarean sections, the NICU, repeat miscarriage, infertility, blood, and possibly more that I don’t even realize right now. I may include pictures sometimes as well. This is my life, as best I can tell it, and I hope it gives a little insight into who I am beneath the sarcasm, emo music, and C-3PO level of know-it-all I carry around the world.
Every Monday, I will post a new part to my own personal birth history. This will not be happy most times, but over the years I’ve given myself a lot more grace and love, and I hope the story reflects that. I don’t know right now how many parts this will have, but it’s going to cover almost a decade of how I truly got to where I am. I’m not going to gloss over hard things, and be aware there is talk of cesarean sections, the NICU, repeat miscarriage, infertility, blood, and possibly more that I don’t even realize right now. I may include pictures sometimes as well. This is my life, as best I can tell it, and I hope it gives a little insight into who I am beneath the sarcasm, emo music, and C-3PO level of know-it-all I carry around the world.
—————————————————————————
I was a Navy brat, moving every couple years, and almost never going to the doctor for anything unless we couldn't fix it at home with time, rest, or OTC meds. I didn't have a distrust of the medical system, more that they were there if we couldn't handle it. I also knew my birth story growing up, along with a lot of my ancestor's stories, something I've learned others didn't have.
I was a cesarean, though my mom planned an unmedicated hospital birth. Most of our family doesn't take any pain meds unless we need them, and birth wasn't when we needed them. My grandmas all had unmedicated births in the 40s, 50s, and 60s, something odd for the time, but for me just made it a given that I would also want and have an unmedicated birth. The pain didn't scare me, even knowing my birth story. My mom didn't have the birth she planned, but she knew anyone could have an unmedicated birth and should try for one.
This isn't to say we trusted anyone outside of a doctor. We didn't see the chiropractor unless it was cheaper to get my physical for sports. We went to our well visits, had our vaccines, used antibiotics for things without question. It was a strange dichotomy to trust them but also not see them.
When I got pregnant with our first, I didn't question the hospital birth. I called the doctor my mom had with me (I was back to living where I was born), found out he retired, and his patients were being seen by the hospital midwife. That felt strange, since I had never seen a midwife, and also was slightly distrusting of them because I had never seen one, but I went along with it. They couldn't get me in until I was 12 weeks, but I figured it I needed anything, they would provide. I knew absolutely nothing about this process, so I accepted everything they said without question.
My friend from highschool, someone I recently reconnected with, had a baby right before I got pregnant. She had him at a birth center, which I thought was insane. Not having him at the hospital? What was the world coming to! He was great, she was great, but that was still a step too far for me. What would happen in an emergency? What if they had died?? She laughed it off, but looking back I know it annoyed her how worried I was about them both. As if she didn't know what she was doing? Compared to me, she was practically a doctor herself with the knowledge she had of the process and what she wanted. Her doing this was absolutely not enough to change my mind on anything, and I blissfully went along with my midwife and hospital experience thinking everything would be great, I wouldn't have issues, and I would have my unmedicated birth whenever my baby was ready to be born.
That was another aspect I learned from my family history - babies are born when they're ready. Induction was a strange topic for us. My grandma, my mom's mother, had a baby way outside her "Due window". They gave her a due date that she didn't agree with, and then stayed pregnant for weeks after her water broke because she knew he wasn't ready to be born. And even when he was born, she knew he was earlier than he should have been. Their dates be damned. So this concept of the body and baby not knowing when to be born and needing to be forced out was so foreign to me. I was "overdue", it was normal, so why rush it?
A lot of this eventually colored my own education and experiences in finding a preceptor, but for my first pregnancy, my wants aligned with the midwife I was seeing, and I didn't question when things weren't how I wanted them, because the end goal - an unmedicated birth - was what we both wanted for me.
I ignored the lack of time with her. When I saw her, it was for maybe 15 minutes, but growing up seeing Navy doctors, that didn't seem odd. Just par for the course. She was excited when we said we didn't want to find out what we were having, she said it was really rare for anyone to choose that and was so excited to tell me at the birth. My choice was colored by two people I knew, my mom and my friend that birthed in the birth center, finding out what they were having just for it to be wrong at the birth. I didn't want that, so finding out was the much easier choice.
We talked about breastfeeding, I knew I could do it because all the women in my family did without issue, and that was that entire conversation.
I did the blood tests they recommended, had my first ultrasound at 21 weeks, drank the horrible glucola drink, and said yes yes yes no matter what.
I told her often that I was still throwing up and sick, and she would laugh and tell me I just needed to want to be pregnant more. "Obviously you just don't want this baby, which is why you're making yourself sick." This was a very wanted baby. I may have only been 19 years old, but it wasn't an accident, even if she thought it was. When I was admitted to Labor and Delivery at 27 weeks with contractions that wouldn't stop and dehydration so severe I needed 3 bags of fluids to even bring my blood pressure up, she still asked why I wasn't bonding with my baby and was making myself sick.
So I stopped talking to her about it. I was slowly gaining weight, though it only ended up being 16 pounds total by her birth, but she was happy with it. I was still spilling ketones and throwing up multiple times a day, but she was happy and I didn't feel like a failure every appointment.
At 35 weeks, I went in for my appointment, got the GBS swap which I was not ready for because they didn't explain anything to me, and then she said "And your baby is head down, things are getting ready for birth, oh wait." She looked at my chart, realized she had never check the baby beyond heartbeat, and had me lift up the gown. She pushed on my belly for a bit, and then said I needed an ultrasound because she thought my baby was breech. Did I understand any of that? Nope. Did she explain? Nope.
I hadn't had an ultrasound since 20 weeks with the anatomy scan. That was my only one up to that point because it wasn't something we wanted or she offered.
So off we went to get a scan. For what reason? We had no idea.
They took pictures, it was really cool to see her, but no one told us anything. I got a call later that afternoon that I was immediately placed on bedrest, that my baby was frank breech and my fluid was low. I had to come in the next day for her to talk to me about what that all meant.
I wasn't worried. I wondered why she sounded worried and panicked, but to me everything felt exactly as it had throughout the pregnancy, and she was kind of overreacting. And yet, I listened. I went into work and put in a leave of absence, my mom came over to help me clean a bit, and I laid on the couch. But not really, because to me it truly didn't seem like an issue so why was I on bedrest? So I was just as active as I had been, rolling my eyes at her the entire time in my mind.
I went in the next day and she explained that my baby's head should be in my pelvis, but instead it was her butt, and on top of that, the ultrasound showed she had no water, and that meant she was not doing well. So I had to have another ultrasound the next day to check on her. Before she even finished these thoughts, she told me she was no longer allowed to be in charge of my care and I was being transferred to an OB I had never met.
Way to bury the lead, lady.
I had an appointment scheduled for later that afternoon with the OB she most referred to, and she would still be involved, but I couldn't see her for my care anymore.
Honestly, not much changed aside from where I went in the hospital to see them. Pee in a cup, sit on the table, take my blood pressure, and wait for them to come in and see me for a few minutes, then go home.
The only difference was this time I was given "choices" of what we could do.
Go to Salt Lake City and hope the University of Utah would deliver her breech, because no one closer could.
Have an external cephalic version (ECV) at 37 weeks and hope her being smaller meant she turned easier and we could go home to wait for labor, while also being transferred back to my midwife if so. If she stayed breech, we try again at 39 weeks.
Have the ECV at 39 weeks which probably wouldn't work because she was bigger, and then be immediately induced if she turned. If she didn't turn, a cesarean that same day.
Schedule the cesarean for 39 weeks without trying anything else.
To say I was blindsided is a small thing. I had no idea what to do. He gave me too many choices without explaining any of them! My mom had a cesarean and came out fine, so should we just do that? Or do we schedule this ECV? The only one that would not happen was driving to Salt Lake. We were poor college kids, my husband had to work, and that just seemed stupid. In hindsight, I wish we had, but that's life.
So we chose option 2. Which is what he wanted us to do. Because if I hadn't asked questions the entire pregnancy, why start now?
We had 3 ultrasounds a week those last two weeks before the ECV. My fluid levels rose, but they were still so worried about it I had to keep coming back. I didn't get why, but again, why start questioning it now.
I got the call the night before the ECV to be at Labor and Delivery at 5am, no foods or liquids after 10pm, and they would get things started.
What you need to understand is that they explained to me the process of getting the ECV, but I didn't truly understand what that meant.
An IV for medications to calm my uterus
An epidural so it didn't hurt
An ultrasound before to make sure she was still breech and then ultrasounds during and after to make sure she was still head down and doing ok
Hooked up to monitors to check her heart rate and to make sure I wasn't (or was) contracting. That depended on who was talking to me, making it super clear. Not.
Cool. Lots of meds, monitors, people, and then my baby would flip and I would go home. No big deal.
I wish it had been.
Gestational Diabetes - Is it an Issue?
Gestational Diabetes or GD is a “syndrome with no risks to mother or baby, and with no symptoms, other than the increased chance of growing a larger than average baby.” -Gail Hart
There is no consensus on GD in pregnancy. Many think it is something that happens depending on the weight of the pregnant person, some say it is just what happens to some people, and others believe that it isn’t real. There are so many variables, and no one truly understands why it happens.
Gestational Diabetes or GD is a “syndrome with no risks to mother or baby, and with no symptoms, other than the increased chance of growing a larger than average baby.” -Gail Hart
There is no consensus on GD in pregnancy. Many think it is something that happens depending on the weight of the pregnant person, some say it is just what happens to some people, and others believe that it isn’t real. There are so many variables, and no one truly understands why it happens.
GD is tested around 28 weeks of pregnancy with a drink called Glucola. It has more sugar than most eat in a day, and then your blood is taken 1-4 hours after you drink it, depending on which test you are taking. The level of glucose in your blood tells them how likely it is that you have GD. If your glucose value is above 140 after one hour, you have to take the three hour test, and if it is too high with that test, you either move to a four hour test or are labelled as having gestational diabetes. Once this happens, you are placed on a special diet to help control your glucose levels, and will most likely be induced early to prevent a larger than average baby at birth.
Midwives are torn on this. The research shows that macrosomia (big babies) doesn’t happen that often with mothers with diagnosed GD, which is the biggest worry when diagnosed. It is very different from a person that has type 1 or 2 diabetes and is pregnant.
During pregnancy, your body is slower to digest sugars, so your fasting glucose level is higher regardless of diet. You swing between high and low more often (one cause of morning sickness), and the normal blood sugar levels are higher. In controlled circumstances of daily urine testing, most pregnant people spill sugar several times during pregnancy, which is normal.
The biggest problem with the GTT (Glucose Tolerance Test) is that the values they are looking for are LOWER than the values given to non-pregnant people. As stated, your sugar levels are higher in pregnancy as a baseline, so why are they looking for lower levels than pre-pregnancy??
In addition, ACOG says that low risk category women do not need to be screened:
Under 25 years old
Not “morbidly obese”
No family history
Not a high risk ethnic group
HOWEVER, even if GD is found, all it is “preventing” is a baby larger than 9 pounds. And even when you are diagnosed with GD, you have a 70% chance of having a baby less than nine pounds, regardless of diet change or insulin use.
Gail Hart theorizes that GD is not a high risk condition, especially if based on failed GTT alone, but in cases where they are having sugar issues in pregnancy, the mother probably was diabetic BEFORE but didn’t notice until the extra strain of pregnancy.
Just because GD doesn’t have symptoms, doesn’t mean that someone with diabetes before pregnancy won’t as well. If they have diabetes mellitus and don’t know, they will have symptoms of:
Excessive weight loss or gain
Extreme thirst
Poly-uria (increased frequency and amount of urine)
Glycosuruia (sugar in urine)
Ketonuria (ketones in urine)
Possible cardiovascular symptoms (leading to high BP)
In pregnancy:
Fundal height large for dates
Baby will be large for dates
Excessive amniotic fluid (hydramnios) is common
A study in Seattle has shown that vitamin c serum levels affect the levels of glucose in the blood, and may affect the development of gestational diabetes.
Someone that barely fails the GTT is also put in the same category of Gestational diabetic same as someone who massively fails the GTT. There is no variance to the label of GD. As Gail puts it, “a temperature of 100.5 is a fever, right? But should we treat the woman with a temperature of 100.5 the same as we treat a woman with a temperature of 105?” That is how GD is treated, anyone that fails the GTT, regardless of how much they are above the limit, are treated the same way in pregnancy, even if they are in fact not diabetic in that pregnancy.
There are alternatives to the GTT:
28 jelly beans and then a blood draw after one hour
Other sugary foods, as long as they equal the amount in the glucola
Using a glucometer yourself to test your fasting, 1 hour and 3 hour levels
If there are no risk factors of diabetes or GD, simply know what the symptoms are and follow up if any occur
There is still not much known about GD, why it happens, who it happens to, and if it is truly a condition of pregnancy.
Resources:
Gail Hart - Research Updates for Midwives
Cochrane database
What's Jaundice All About?
Jaundice in the postpartum period is the name for the yellowing of a baby’s skin and eyes in the newborn period from the breakdown of red blood cells the liver is unable to handle due to immaturity. Since yellow is not a normal color for a human, it can make doctors and parents very nervous, especially if it continues and worsens over the first week of life.
Jaundice in the postpartum period is the name for the yellowing of a baby’s skin and eyes in the newborn period from the breakdown of red blood cells the liver is unable to handle due to immaturity. Since yellow is not a normal color for a human, it can make doctors and parents very nervous, especially if it continues and worsens over the first week of life. Jaundice is a physiologic response in the newborn’s body to the adjustment from womb to world, as the liver learns how to work and process the excess red blood cells. It’s normal for it to begin around day 3 postpartum, and can last longer if the milk is delayed in coming in if breastfed, or if a baby hasn’t been eating in the first few days postpartum, like during a NICU stay.
There are times when jaundice is not normal and can indicate a very sick baby, like if it happens before the baby is 24 hours old, or if it spreads to their feet. Jaundice coloring starts in the face, normally the eyes are the first to start changing, and then it travels down the body if it progresses, normally only to the chest before it starts to go away. This does not mean the baby is sick, it means that the newborn’s body is normal and going through a process to get its body to work on its own.
The fetus, or baby before it is born, has a completely different system of circulation than the baby once it is born and breathing on its own. Blood doesn’t circulate through organs and the body in the same way in the womb as it does out of the womb. So your baby is not only coming out of a warm, quiet, dark environment, but they are also going through a huge change in how their body works at the base level.
To test bilirubin levels, the amount of red blood cells in the body that the liver has yet to filter and remove, a blood test is required. It is a heel prick on the baby and blood is collected to see the level and decide if treatment is necessary, if the levels are rising or falling, and to have a scientific picture of what is happening inside the baby’s body. Many doctors will require the baby to be under bililights, to help the body get rid of the build up of bilirubin, even if the baby is healthy and fine. The lights make babies tired, so they have a harder time waking up to eat, which can be a reason for the higher build up of bilirubin since their body isn’t going to have as much energy and food to poop out the excess once the liver processes it.
Yet here is the thing beyond the scary - jaundice is protective! It’s an antioxidant, preventing cell damage of the brain and liver among other organs, it prevents damage to oxygen and fat cells, and it prevents premature babies from eye disease. It is also a way for the body to protect against bacteria! Which is really helpful for premature babies, which have a higher rate of jaundice than full term babies. Another neat thing is that vernix, the incredible white frosting covering most babies, helps lower jaundice levels, as yet another reason to delay their first bath and let them be in their own body for awhile before intervening. Which is really cool!
There are a lot of things we know about why some babies get jaundice more and why others don’t, but there is also a lot we don’t know about why physiological jaundice happens. Male babies are more prone to jaundice than girl babies, just like premature babies are more prone to jaundice than full term babies. Any drugs the mom is given in labor will affect the jaundice of her baby because it makes her liver more overloaded to cleanse the body, same with drugs given to the newborn.
Dr Jack Newman, a doctor in Canada that is an incredible resource for breastfeeding, says that jaundice is a breastfeeding problem. If your baby isn’t nursing well, if they aren’t clearing their bowel because they aren’t eating well, the buildup of bilirubin in their gut will lead to jaundice, sometimes higher levels than would happen if the baby ate well right from birth. If your baby nurses well right from birth, they will clear out the bilirubin quicker than a baby that doesn’t, maybe appearing to not have jaundice at all, or a very mild case. It’s also helpful to know that if your baby isn’t nursing well and has jaundice, it’s best to get breastfeeding help as soon as you can, to help not only with the jaundice, but your breastfeeding relationship.
Jaundice doesn’t need to be scary. In many ways, it’s a normal part of life for a newborn baby, and we overthink it. And in the medical world, they see many more sick babies than midwives do, and their thought process goes to those babies and not normal healthy babies that are 100% fine regardless of their yellow face and chest.
Resources:
Taking Back Birth Podcast - Why Jaundice Freaks Out Doctors and How to Protect Your Baby Anyway
Dr Jack Newman
Miscarriage Series - Part 5
Part 5 of my miscarriage series - three meditations to help with the release of the pregnancy, grief, and a message of hope.
This part five of a five part series, based entirely on miscarriage. It will talk about signs and symptoms of miscarriage, physical health, medical care, holistic care, physical healing, emotional healing, memorials, how to help a friend of family member, and will have three meditations available to listen to.
In my shop there is a document with every handout in one file, if you want to download them that way instead of individually from each post. There is a small fee for this to help with costs. The posts and handouts on each post are available for free, though donations are appreciated for the work to create this resource and also to help those going through a miscarriage. Links to donate are available at the end of each post.
——————
Meditation #1: To help with the physical release
Meditation #2: Feeling all you need to feel
Meditation #3: A Message on Hope
——————————————
If you wish to donate to my business to help those going through miscarriage, you can below as well. I offer holistic loss services as donation based fee only.
Miscarriage Series - Part 4
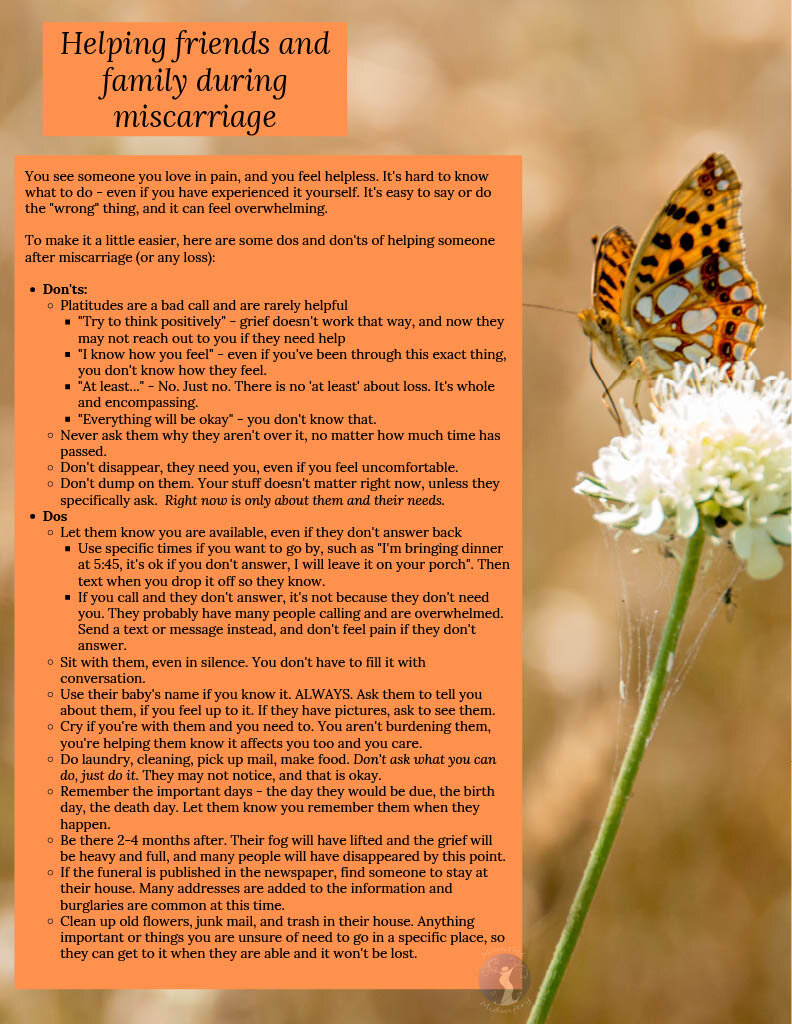
Part 4 of the miscarriage series - How to help friends and family after a miscarriage.
One of the hardest parts many find is how to be there for someone they love while they are going through a miscarriage without being a burden or saying the wrong thing. I wish I could say that you will never say the wrong thing or that you will be the perfect support. Life isn’t that easy. But there are many things you can do to make sure you are helping them through the pain instead of adding to it. Don’t be afraid to be with them, your disappearance can be just another thing they’ve lost. If you learn anything from this let it be this one thing - don’t leave them.
This part four of a five part series, based entirely on miscarriage. It will talk about signs and symptoms of miscarriage, physical health, medical care, holistic care, physical healing, emotional healing, memorials, how to help a friend of family member, and will have three meditations available to listen to.
In my shop there is a document with every handout in one file, if you want to download them that way instead of individually from each post. There is a small fee for this to help with costs. The posts and handouts on each post are available for free, though donations are appreciated for the work to create this resource and also to help those going through a miscarriage. Links to donate are available at the end of each post.
——————
One of the hardest parts many find is how to be there for someone they love while they are going through a miscarriage without being a burden or saying the wrong thing. I wish I could say that you will never say the wrong thing or that you will be the perfect support. Life isn’t that easy. But there are many things you can do to make sure you are helping them through the pain instead of adding to it. Don’t be afraid to be with them, your disappearance can be just another thing they’ve lost. If you learn anything from this let it be this one thing - don’t leave them.
It can be daunting to face death, especially of a baby. Babies aren’t supposed to die. Babies are supposed to live, bring us joy and laughter. Death doesn’t do that. And so often, the way we get through death is remembering times when they did bring us joy, yet in miscarriage that isn’t really a possibility. There aren’t birthdays to remember, milestones, memories of smiles. There is just a hole.
There is a really great idea that grief and holding space are about circles. It’s called The Ring Theory, and it beautifully applies to miscarriage.
I’m going to quote from the author of this theory:
The person in the center ring can say anything she wants to anyone, anywhere. She can kvetch and complain and whine and moan and curse the heavens and say, "Life is unfair," and, "Why me?" That's the one payoff for being in the center ring. Everyone else can say those things too, but only to people in larger rings.
When you are talking to a person in a ring smaller than yours, someone closer to the center of the crisis, the goal is to help. Listening is often more helpful than talking. But if you're going to open your mouth, first ask yourself if what you are about to say is likely to provide comfort and support. If it isn't, don't say it. Don't, for example, give advice. People who are suffering from trauma don't need advice. They need comfort and support. So say, "I'm sorry," or, "This must really be hard for you," or, "Can I bring you a pot roast?" Don't say, "You should hear what happened to me," or, "Here's what I would do if I were you." And don't say, "This is really bringing me down."
If you want to scream or cry or complain, if you want to tell someone how shocked you are or how icky you feel, or whine about how it reminds you of all the terrible things that have happened to you lately, that's fine. It's a perfectly normal response. Just do it to someone in a bigger ring.
"Comfort in, dump out.”
Illustration by Wes Bausmith
The person most affected by this is the pregnant parent. The next is their partner. You are not in the center ring in this situation - EVER. You are in a larger circle than them. You need to dump all of that out to a larger circle. It isn’t about you.
This one thing is so important to remember. Be there, and comfort in, dump out.
Now, don’t let this intimidate you. It’s scary. And even as someone that has been through repeat loss, I say the wrong thing sometimes. All we can do is try not to do it again, and be aware of what we are doing. It’s that simple.
As for don’ts - this is HUGE. And a big part of this I’ve already written about. DO NOT LEAVE THEM. Be there. Check in. Don’t expect answers back, but make sure they know you are there. They aren’t ignoring you, because it isn’t about you. They are dealing with this the best they can, and they deserve your love and trust.
Platitudes are gross. Try really really really hard to never use one. They feel impersonal, and to some can even feel like an attack.
These include:
“Try to think positively” - positivity can suck it. Grief isn’t a bad thing and positivity isn’t the answer.
“At least…..” - THIS ONE SUCKS. There is no at least about miscarriage. It’s whole and encompassing, and at least diminishes it.
“I know how you feel” - remember: COMFORT IN, DUMP OUT
“Everything will be okay” - you don’t know that.
Never ever ever ask if they are over it. Even if it’s 50 years from now. No one would ask someone if they were over their partner dying, so don’t ask it now. The loss mattered, their grief matters.
Don’t disappear. In 2-4 months, things will get much worse for them, and they will need everyone they can.
Don’t dump your crap on them, unless they ask and seem truly interested
Again, don’t be intimidated. Keep showing up, even if you stick your foot in your mouth. In the end, when the fog lifts and their grief is a little smaller, they will remember that you were there. That’s so important.
I figured I would end the post with practical tips on how you can help, and know that even if you can’t do any of these because of distance or personal stuff or any other reason, that’s okay too.
I know I’ve repeated this numerous times in this post, but let them know you are there. If you are available in person, let them know specific times you will be by. Things such as this:
“I’m bringing dinner by at 5:45. You don’t need to answer the door, I will leave it outside if you don’t answer. I will text/call when I get there to let you know.”
“I’m coming by on my lunch break at 1pm, I would like to do some laundry or clean for you. If you’re okay with that, leave the door unlocked or answer when I knock. If you aren’t, that’s ok. I’m available if ever you are.”
If you call or text and they don’t answer, this is not a reflection on you. They are going through something and sometimes it’s just too hard to even wake up, let alone talk to people. Know that it isn’t about you, and they appreciate the reaching out.
Sit with them, in silence if they don’t want to talk. You can’t fix this with words, but your presence can be a comfort.
ALWAYS USE THEIR BABY’S NAME IF YOU KNOW IT. This is the biggest thing you can do with your words. USE THE NAME ALWAYS. You aren’t reminding them, you aren’t making them sad, you are agreeing and showing you loved that baby as well. You are giving them a gift by acknowledging the life that existed.
It’s okay to cry if you are with them. Seeing someone else have big emotions can help them express their own.
Do something whenever you visit
Pick up trash, take the trash out, do the dishes, do laundry, vacuum, cook for them. Anything!
They may not notice things that need to be done, but even if they do, these little acts of physical love are important so they know they aren’t forgotten, and it will lighten their load just a little.
They may not even notice you did it, AND THAT IS OKAY. It’s not for them to say thank you and show gratitude right now. It’s for you to put comfort in. That’s it.
If you pick up mail or anything else, whether from a mail box or inside the house, make sure to put it in a central location that they know about. Bills can be forgotten in this time, and no one wants their power shut off because they don’t remember getting a bill.
Remember the important days
The day they died, the day they were born, their due date, first birthday. Those days matter in the years to come. One of my most treasured things is someone remembering their birthday. It doesn’t happen often, yet every time it does it is one of the most amazing feelings.
If the funeral (if there is one) is published in the paper, have someone stay at their house. Burglaries are common during this time, and having someone at the house can ease the parents’ mind so they can grieve and say whatever they need to without worry.
Small things in this time matter. One day they will wake up and things will be a little clearer, and when that happens, you don’t want to miss it because you walked away. When they laugh for the first time, when they want to go out to dinner or a movie, when they want to do something - you want to be there for those. There is no guarantee that every day will be good once that starts, because grief is like an ocean wave - coming and crashing against you when you least expect it. Be there for the good and the bad - it matters.
A very dear friend Kristine Brite McCormick wrote a wonderful booklet titled “When Your Friend’s Baby Dies”. Her daughter Cora died at 5 days old, and after many missteps and people asking what they could do since they had never been in this before, she wrote this to help. It’s 24 pages long, and worth the purchase and read.
You get a text message or voice mail you'll never forget. Your friend's child has died. You want to help, but you're afraid of doing something wrong or overstepping your bounds. Kristine Brite McCormick, who lost her baby at five days old to a heart defect, guides you through some suggestions for helping your friend and gives you the insight from her experience as a babyloss mother in this booklet. This short and easy read offers practical tips about how to help after your friend's baby dies and also gives you an insight into what your friend might be feeling.
In the end, remember the one thing - just be there. It truly matters.
—————
Below is the one handouts as an image file that is free to download. Simply click the image to be taken to the file. If you wish to have higher quality PDFs, please visit my store for the file containing every handout in this series.
If you need a coupon code or the files for less than the $10 they sell for, please reach out to me.
If you wish to donate to my business to help those going through miscarriage, you can below as well. I offer holistic loss services as donation based fee only.
Miscarriage Series - Part 3
Part 3 of my miscarriage series - this one about emotional healing, grief, and creating something to remember your baby.
This part three of a five part series, based entirely on miscarriage. It will talk about signs and symptoms of miscarriage, physical health, medical care, holistic care, physical healing, emotional healing, memorials, how to help a friend of family member, and will have three meditations available to listen to.
In my shop there is a document with every handout in one file, if you want to download them that way instead of individually from each post. There is a small fee for this to help with costs. The posts and handouts on each post are available for free, though donations are appreciated for the work to create this resource and also to help those going through a miscarriage. Links to donate are available at the end of each post.
——————
In part one I wrote what a miscarriage is and how it can happen, and in part two I wrote about medical care, holistic care, and how to help your body physically through a miscarriage. Those are things not talked about enough, as miscarriage is seen as shameful (only to ourselves, rarely ever do outside people think that).
So now that the physical is out of the way, let’s dive into the emotional. No one likes discussing grief and emotions, yet so much of miscarriage is tied to this, especially after it happens.
I’m sure most are aware of the Five Stages of Grief. It’s not something that I really think applies! Sure, there are five stages, but in grief, you don’t calmly go from one to another; you jump around. One day you may wake up and be completely okay with what happened, and then the next be a ball of anger that nothing can calm. It’s a process, and most times it lasts forever. Grief is the price of love.
This is one of my favorite graphics on grief, mostly because it perfectly explains what I went through. Yes, some may not grieve this way, but it’s still important to know if that isn’t you, because others might. Grief isn’t a straight system, it’s complex and messy and confusing.
None of this to say there isn’t help out there or ways to make the process easier! You do need to feel the emotions and grief, to find a place to put the love you had for the baby you couldn’t keep, even if you didn’t plan to keep it, because your body remembers everything.
It may seem out there, thinking of your body having memories, your body grieving even if the outcome was something you wished for, but there is a lot of evidence out there that muscle has memory, your body feels things that you may not realize were an issue, and we hold onto hard things without meaning to. Phantom limb pain, driving a car without thinking about how you’re doing it, being awake yet seeming to do things without being aware. All of those are signs your body knows what is happening even when your conscious mind doesn’t.
There are many options to help your grief and your emotions, though I will only go through a few:
Support groups, Community Care, and Online Resources
These can be in person, online in groups or message boards, over the phone, on zoom (since this is the way everyone is communicating currently!). You don’t have to do things in person to get the support you need during and after a loss.
There are a lot of amazing online resources, many of which I used myself when going through repeat miscarriages. Things have changed over the last decade, but they are still available and can be a wonderful way to get a friendly shoulder if you don’t want to tell those in your family what is going on.
Stillbirthday - Heidi has created a wonderful resource for all phases of loss, with birth plans, support groups, information, and more resources to help you find whatever you need to get through.
She also does a heart release every year, writing names of thousands of babies by hand, for free. Heart Release
Still Standing Magazine - A ton of resources on all stages of loss, including LGBTQA+, and an online free support group
Grieve Out Loud - The facebook page is also a great resource, with a free online support group. Their penpal program is one of the coolest parts of what they do. Years ago in the midst of everything, I was one of the penpals. I had five or six people I wrote to to check on, and also had a penpal for myself to write to when things were really bad. The way that loss parents love each other is such a wonderful part of a heartbreaking community.
They also have a massive resource page
If you are a health care worker, PLIDA is for you. The Pregnancy Loss and Infant Death Alliance is a formal network to increase awareness and training for loss support.
Share is a national organization for pregnancy and infant loss. They have chapters set up all over the country, and provide information and resources for families, providers, and those going through a loss. Most chapters have their own support groups.
Therapy!
This is not a bad word!! It is not wrong to need extra help from a professional. Money may be an issue for this, and many offer cash prices if you do not have insurance, and it can make a huge difference in your healing.
There are many kinds of therapists, and some even work solely online. It’s okay to take your time finding a good fit, and even if it’s just sporadic care, it can make a big difference.
Try to find one that is trained in grief, loss, trauma, if possible. If not, find one you fit with.
Self-Care
This does not need to be expensive spa days! It can be something as simple as eating a meal every day.
One of the pictures or PDFs is a self-care checklist, very simple things to make sure you are taking care of yourself in a hard time. It can be hard to remember to eat or drink, and showering may be too hard and require too much effort. All you can do is try, and that’s enough.
For many, there is nothing to remember their baby or pregnancy - not even stretch marks. You didn’t buy clothes, you didn’t make anything, you didn’t have anything to keep from the physical loss, and many may not even know you were pregnant and had a miscarriage. It can be hard to feel emotions when there is nothing tangible to grieve. This is where memorials come in.
Some cemeteries will allow the formal burial of any human remains, regardless of gestational age. They are more rare, and many states won’t allow burial before 20 weeks, or after the age of miscarriage. It sucks, and in turn makes cemeteries hard places for those without that physical place to go to grieve their loss. If this is something you want, many cemeteries will work with you, even letting you use other plots you own, like grandparents, and bury remains in the same place. Some even allow you to dig your own hole and have your own plot for a very small fee. The worst that can happen is they say no, so if you are wanting this, reach out.
Having a ceremony can be a healing experience
This can be something as simple as having friends and family meet at a neutral location like a park, and release flowers or seeds or balloons.
However, if you are considering a balloon release, please know that it affects the wildlife in your area, and can kill them. Balloons are a wonderful way to celebrate life, but a release comes at a cost.
I’ve been to a few where we have a sort of wake and eat food and just enjoy each other. I’ve also been to others where it is a more formal ceremony, with note writing, memories given, feelings shared, and lots of tears. It’s 100% up to you to have or not.
Food is one of the best ways to remember. Mostly because it opens us up, gives us something to do instead of just talk and feel. You can find a special dish or something you craved during pregnancy, and every time you eat that or have that or even just see that, you remember your baby.
In line with that, picking something special to remember your baby can be such a healing thing.
Memorial necklaces, keychains, paintings, and more are all options. Etsy has hundreds of people that make them, and they feel personal and filled with love.
Pick an animal or object or shape that relates to your baby or you feel embodies your baby. My earlier losses I feel connected to them when I blow wishes, or the dandelion seeds. Two others are a when I see a blue dragonfly or a butterfly. A dear friend sees swirls around and knows that’s her baby saying hi. I read a thing years ago that said that every time you see a coin on the road it’s your baby saying hello. It can be anything. And you don’t have to tell anyone, it can be secret to you.
—————
Below are the three handouts as image files that are free to download. Simply click the image to be taken to the file. If you wish to have higher quality PDFs, please visit my store for the file containing every handout in this series.
If you need a coupon code or the files for less than the $10 they sell for, please reach out to me.
If you wish to donate to my business to help those going through miscarriage, you can below as well.
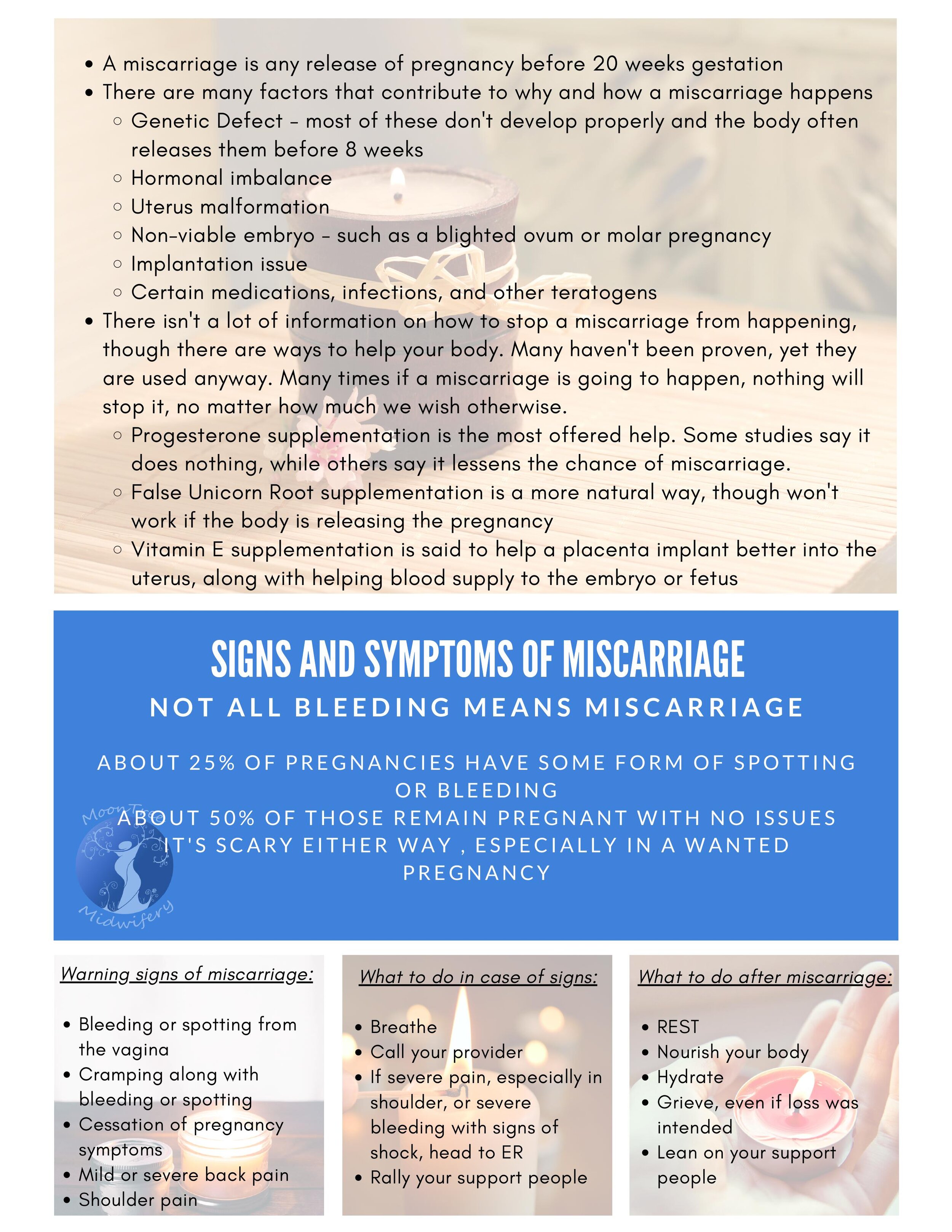
Miscarriage Series - Part 2
Part 2 of my miscarriage series, with information on medical and holistic care, along with how to care for your body physically.
This part two of a five part series, based entirely on miscarriage. It will talk about signs and symptoms of miscarriage, physical health, medical care, holistic care, physical healing, emotional healing, memorials, how to help a friend of family member, and will have three meditations available to listen to.
In my shop there is a document with every handout in one high quality pdf file, if you want to download them that way instead of individually as jpgs from each post. There is a small fee for this to help with costs. The posts and handouts on each post are available for free, though donations are appreciated for the work to create this resource and also to help those going through a miscarriage. Links to donate are available at the end of each post.
—————————
In the last post I talked about the physical side of normal miscarriage, along with definitions and signs of complications. It is a very basic overview of miscarriage, and in this post we will dive into the different types of care you can receive during your miscarriage, along with how to help your physical body during and after a miscarriage.
In the US, medical care given by doctors is the standard or normal for many people. Some prefer more natural means, but the majority will seek medical care before, during, and after a miscarriage, if only because that is what they are used to. Most obstetricians have to take extra classes to handle miscarriage care, and a lot of them never do this. It isn’t required to become an OBGYN. Their training is more focused on pregnancy and term delivery and all that can go wrong during that time. It’s mostly about control of what you can control.
You may not have time to think through your options before your miscarriage begins, or you may have some extra time in the case of a missed miscarriage. It is so unique to each person.
If you are interested in medical care for your miscarriage, there are a few options that you need to be aware of, since no miscarriage is handled the same as another. You are ultimately in control of the situation, even in emergencies.
The very first thing many providers will do if miscarriage is suspected in early pregnancy is order a blood draw to check your HCG levels, to be repeated in 48 hours. HCG is the hormone created when implantation occurs, and it doubles in value every 48 or so hours in normal healthy pregnancy. It never drops if everything is okay, it only goes up. The second value is the most important one because of this. One lab draw by itself can only show if you are pregnant or not, it does not say what is going on with the pregnancy. These values also become more stagnant in their rise the farther along in pregnancy, so if you are farther than 6-7 weeks, they will only show a rise or fall, nothing else related to how the pregnancy is progressing.
If you are farther than 6 weeks, many will then schedule or perform an ultrasound to check on the embryo and the uterus. Sometimes this is done before the labs are drawn, sometimes it has to wait until after. It is truly up to you and your provider. If you are less than 6 weeks, it is very unlikely to see any sort of embryo in the ultrasound, and definitely not cardiac activity. If you are earlier than 5 weeks, you may not see anything in the uterus. Knowing your dates is one important piece to getting an ultrasound at the right time, and it might be best to wait if you can to get that ultrasound.
If both or either of these are done, most providers will then wait and see before next steps, even in the case of missed miscarriage. In the case of earlier miscarriage before 10 or so weeks, they will give you the option of waiting a week or two before coming back in for more tests and then medication or surgery to end the pregnancy. Sometimes they will give you the option that day to do either of those things, but it’s not as common.
From here, you have three options.
Wait and see. Your body will probably start labor on its own and pass the contents of your uterus within a month. It can take time, and when you found out your pregnancy isn’t viable, it can be really hard to wait for the end date. For many, they need that release to start healing, and until that occurs, they live in limbo.
Medication options
The first option is mifepristone. This is a progesterone blocker, normally used in abortion, but also used if the fetus is no longer growing properly or miscarriage is imminent but the body hasn’t realized it.
The second option is misoprostol, or cytotec. This is a contraction inducer, starting the physical release of the pregnancy. This is taken at home either orally, rectally, or vaginally.
With either of these options, the embryo or fetus should pass vaginally, and you can keep the remains to do with what you will.
Surgical options
A D&C or D&E (depending on length of pregnancy and what needs to be done to clear out the uterus) is performed under sedation or general anesthesia. General is not common, sedation is the more used anesthetic.
Your cervix is dilated, and a curettage or vacuum is inserted into the uterus to clean out the contents.
In this option, you cannot keep the remains, as they have been pulled apart by the tools.
Regardless of what you choose, there are positives and negatives to each. Medication options could mean that the uterus releases its contents but leaves some behind, meaning you will need surgery anyway. Surgery comes with its own risks, and it is also possible that the uterus isn’t completely cleaned out, and you will need another one. Regardless, you will have vaginal bleeding for days or weeks after, as your body sheds your uterine lining and goes back to its pre-pregnancy state.
Now, there are those that don’t want a medical option for their miscarriage, for whatever reason. It’s 100% your call which way to go. If you don’t wish to have medical intervention, there are many options to go through.
Nourishing your body physically and emotionally during the wait. This includes getting enough food and water, along with proper rest. Your body can’t work if it isn’t being taken care of, and having a miscarriage is a lot of work. One of the best ways to nourish your body is through herbs, especially in teas and tinctures.
There are many to choose from: Red Raspberry Leaf, Ginger, Peppermint, Motherwort, Nettle, Red Clover, Echinacea, and Elderberry
It’s okay to take as long as you need. As long as you don’t have heavy bleeding and hemorrhage or signs of infection, time is on your side. Sometimes it can take a month or more for the body to catch up if left on its own, and that is not an abnormal amount of time.
In the Holistic Care Handout I have added three sections on the left side that deal with herbal ways to proceed with a pregnancy release. If you are thinking of going this direction, all you need to do is pick one thing from each section, using them from the top to bottom a few days or a week before moving on to the next section. Most of the items can be found without issue locally, regardless of where you live. They can also be used if you are in the physical process of the miscarriage and want to speed it up or aid the process.
Sometimes in this place, your body needs only one thing from you - acceptance. Not to put off grief or anything else, but to understand and feel that the miscarriage needs to happen, and that you are physically holding on through your emotions. In part six there will be a meditation for releasing the emotions and the pregnancy. Intention can be a very big part of this process. Your thoughts and feelings matter.
Now that you have figured out which way you want to go, or simply know your options on how to proceed, one of the most important things to consider during and after miscarriage is supporting your physical body. Your body has gone through pregnancy and birth, even if it isn’t what you hoped. Even being pregnant for a short time, your body went through hormonal, mineral, vitamin, and other physical shifts. During the actual release, you lost blood and other nutrients that your body needs to heal optimally and remain healthy.
One of the biggest things to do is get adequate rest. If you are constantly going, it’s hard for your body to relax, and you need to sleep to heal. Your body went through a process and needs the rest, even if it is just sitting down for an hour or two. Many workplaces won’t give sick or vacation time after a miscarriage, so take whatever you can get and relax your body.
You also need to eat well. You need to rebuild your iron levels, your blood stores, and your nutrient and vitamin stores. This is important even if you aren’t considering pregnancy again in the near future. What you do during this postpartum time matters for the next years. In Ayurveda, they say that what you do for the next 40 days affects the next 40 years.
Lastly, you need to stay hydrated! Not with soda, with water. You have to drink water. It can help prevent and alleviate headaches and migraines, exhaustion, depression, and anxiety.
—————
Below are the four handouts as image files that are free to download. Simply click the image to be taken to the file. If you wish to have higher quality PDFs, please visit my store for the file containing every handout in this series.
If you need a coupon code or the files for less than the $10 they sell for, please reach out to me.
If you wish to donate to my business to help those going through miscarriage, you can below as well. I offer holistic loss services as donation based fee only.
Miscarriage Series - Part 1
Part 1 of a series specific to Miscarriage.
Miscarriage is defined as any pregnancy release before 20 weeks gestation. This could be something as early as 3 weeks all the way to 20 weeks of pregnancy. Because so many things happen during this time in pregnancy, it can seem really odd that they are defined by the same word, but welcome to science. It is also a word that many people hate, as if you missplaced your pregnancy, as if it was under your control.
This part one of a five part series, based entirely on miscarriage. It will talk about signs and symptoms of miscarriage, physical health, medical care, holistic care, physical healing, emotional healing, memorials, how to help a friend of family member, and will have three meditations available to listen to.
In my shop there is a document with every handout in one file, if you want to download them that way instead of individually from each post. There is a small fee for this to help with costs. The posts and handouts on each post are available for free, though donations are appreciated for the work to create this resource and also to help those going through a miscarriage. Links to donate are available at the end of each post.
———————————————————
Miscarriage is defined as any pregnancy release before 20 weeks gestation. This could be something as early as 3 weeks all the way to 20 weeks of pregnancy. Because so many things happen during this time in pregnancy, it can seem really odd that they are defined by the same word, but welcome to science. It is also a word that many people hate, as if you missplaced your pregnancy, as if it was under your control.
For many people, this is a loss of a wanted pregnancy. For some it isn’t, and for others it is the wanted end of a pregnancy. There are many emotions beneath the surface, and one person’s experience isn’t the same as another’s, even if they happen at the exact same gestation and in the same way.
There are many types of miscarriage, depending on how far along the pregnancy, lab values if labs are taken, ultrasound results, and how the pregnancy is growing or not growing. Some basics to miscarriage types are:
Missed Miscarriage - when an embryo or fetus stops growing, but there are no outward signs of issues. Most of these are found either through routine ultrasound or when the miscarriage begins without other signs and symptoms of something amiss. Most missed miscarriages are treated with medical care, as waiting for the body to catch up and begin the process can be hard and longer than a few days.
Chemical Pregnancy - A pregnancy that progresses in chemical and hormone only, most often released before six weeks gestation. You may get a light positive test, followed by negative tests, or no positive tests at all if your hormone levels are not high enough, but have a period different than others.
Blighted Ovum - A fertilized egg that never develops and embryo or fetus. Ultrasounds in this case show nothing more than an empty sac. You may have all the symptoms of a healthy pregnancy, as the body is still supporting the growth of the sac. Sometimes in this case the only way to release the ovum is with medical or herbal means.
Molar Pregnancy - A fertilized egg continues to divide and grow, not becoming an embryo or fetus. It some cases, it can become a type of cancerous cell, and leave behind parts of itself and can affect future pregnancies. Care of a known molar pregnancy are specific and medical, though the chance of a molar pregnancy are very low and it is more rare than other types of pregnancy.
Ectopic pregnancy - Any embryo that does not implant into the lining of the uterus, though most often implantation occurs in the uterine tubes. If it is undiagnosed, it can lead to a tubal rupture, and emergency surgery is required to stop the bleeding. If a pregnancy implants anywhere outside the uterus, the odds of the pregnancy continuing are very slim, and planned release and/or surgery are necessary to save the life of the pregnant person. There is no way to reimplant an ectopic pregnancy.
In most cases, miscarriages happen before 8 weeks gestation, or one month after your missed period. The majority of these are caused by a genetic defect in the fertilized egg, and nothing you did caused it. The chances of miscarriage before 8 weeks are around 1 in 4, after 8 weeks, it lowers to around 5% of pregnancies. After 12 weeks, or when most feel comfortable announcing their pregnancy, the chance of miscarriage drops to around 1%. This isn’t to say it doesn’t happen, just that the chances are smaller than before.
In general, no one truly knows why miscarriage happens. There are times when it’s genetic and the cause can be found, but sometimes miscarriages just happen, though no fault of anyone. With the routine use of early ultrasound, more missed miscarriages are being found, leading to an increase in miscarriage numbers, when 50 years ago most wouldn’t even know they were pregnant at that point.
No matter the cause, miscarriage is hard. It’s hard physically and emotionally. The body goes through a hormonal shift, which causes an upheaval, even if the pregnancy wasn’t desired or tried for. Being prepared for the physical and emotional aspects of miscarriage, even after the fact, can help ease the adjustment and transition.
The physical signs of miscarriage include, but are not limited to:
Spotting or bleeding, with or without cramping
Back pain
Shoulder pain
Cramping, even without bleeding
Abrupt cessation of pregnancy symptoms
Sometimes everything can seem like it is going well and fine and the next minute you could be in labor and miscarrying the pregnancy. There is no rhyme or reason to why it happens. In general, most miscarriages resolve on their own, with no need for outside help or physical preparation. However, with early ultrasound being more routine, many more people than before are aware a miscarriage will happen before the body is prepared for it to begin.
If a miscarriage begins without prior knowledge, the most important thing is to stay calm and monitor your body. Keep an eye on your bleeding, take pain medication such as tylenol if needed, and make sure you feel okay. Some say that a miscarriage is just a heavy period, and for some that is accurate, but for others it can be very painful and the bleeding heavy enough to be worrisome.
In general, there are many guidelines to follow if you are going through a miscarriage or planning on going through a miscarriage.
If you have heavy bleeding of more than one heavy pad in an hour, the pad completely saturated, you could be bleeding too heavily and need assistance.
If you have severe and persistent abdominal, back, or shoulder pain, it could indicate infection or internal bleeding and you need to get medical assistance as soon as you can.
Labor during a miscarriage will proceed fairly normally, without any outside help, from lighter bleeding and cramps to more intense and heavy bleeding and stronger cramps and contractions. The bleeding and pain will normally peak with the release, and then both will taper off over the next days. You will bleed for a few days or weeks after, as the body is releasing the lining created during the pregnancy. Even if you have a surgical release, the bleeding will continue.
Blood clots and bits of tissue are normal parts of a miscarriage, and unless the blood clots are larger than the size of an egg or you feel funny or weak, are nothing to worry about.
If you notice any signs of infection, such as foul smell, sharp abdominal pain, or strange colored discharge, getting medical help may be the best option to make sure it doesn’t spread.
Sometimes milk comes in after a miscarriage, though it’s more common for this to happen after 20 weeks of pregnancy. Stillbirthday has a great resource (written by me) on lactation after miscarriage, and I won’t recreate the wheel for you here.
——————
Below are the three handouts as image files that are free to download. Simply click on each to be taken to their file page. If you wish to have higher quality PDFs, please visit my store for the file containing every handout in this series.
If you need a coupon code or the files for less than the $10 they sell for, please reach out to me.
If you wish to donate to my business to help those going through miscarriage, you can below as well. I offer holistic loss services as donation based fee only.
Close to the Bones Episode #6
I want to talk a bit about why I saw an OB early and often in pregnancy until I decided to stop.
Close to the Bones Episode #5
In which I talk about the power of telling your story to those that are holding space for you, along with sharing the good stories for others to hear, along with a new offering for my community!
Close to the Bones Episode #4
TW: pregnancy loss, ER, hemorrhage, OB, ‘products of conception’. In which I talk about one of the hardest days of my life.
Body Image and Pregnancy Weight Gain
Our society is so fixed on the ideal body type - skinny, fit, active, toned. No one wants to gain wait, to be “obese” based on their BMI, and there is so much focus on not gaining weight or only gaining appropriate amounts of weight that we can’t seem to discuss weight gain in pregnancy without someone leaving the conversation feeling inadequate. The recommendations for weight gain in pregnancy seem to change constantly, with diet recommendations changing almost as frequently. And it makes you wonder, does body image insecurity feed into pregnancy weight gain and what can happen because of it?
Our society is so fixed on the ideal body type - skinny, fit, active, toned. No one wants to gain wait, to be “obese” based on their BMI, and there is so much focus on not gaining weight or only gaining appropriate amounts of weight that we can’t seem to discuss weight gain in pregnancy without someone leaving the conversation feeling inadequate. The recommendations for weight gain in pregnancy seem to change constantly, with diet recommendations changing almost as frequently. And it makes you wonder, does body image insecurity feed into pregnancy weight gain and what can happen because of it?
The social pressure to be thin and fit is far reaching. Even small children are picking up on this and wanting to be thinner. Weight Watchers even created a new program for kids, as if any child needs to be on a restrictive diet! Weight is such a tender topic, and so many are blaming the body positive movement for the rise in obesity, when there are many other factors at play. However, in pregnancy, weight gain should be the normal for every pregnant person, regardless of weight before pregnancy, and it can lead to a lot of heavy emotions and some people even end up diet restricting so they gain inadequately or not at all, and in some cases, even lose weight.
Even with that, this is the first time in many people’s lives that they are encouraged to gain weight, which is at odds with what they’ve been told their entire life. It can be hard to change your mindset around weight gain, even when you want to do everything possible to have a healthy pregnancy and healthy baby. A paper published by the WHO states, “During pregnancy and postpartum, women’s dissatisfaction with their bodies increases irrespective of how satisfied they were prior to the pregnancy. Evidence suggests that pregnant women who are affected negatively by changes to their body are less likely to initiate breastfeeding.” ¹ The breastfeeding aspect was a huge shock to me, I hadn’t thought of the connection to body image with the rates of breastfeeding or even just the initiation of breastfeeding. And the bit before that about stating that it didn’t matter how satisfied they were before pregnancy, the dissatisfaction with their body increased as pregnancy progressed.
A study published in 2009 about prepregnancy BMI, gestational weight gain, and likelihood of major depressive episodes discusses the impact of weight gain on incidences of depression during pregnancy.² Their findings weren’t very shocking, even with the body shaming attitude of obesity and BMI, and they showed that all sized people had an increased risk and chance of depression in pregnancy, though the risk was higher with those classified as “obese” before pregnancy. Interestingly enough though, those that were normal BMI before pregnancy had a much higher chance of depression if they had inadequate weight gain during their pregnancy. It almost feels like a doubled-edged sword - gain weight and it’s an issue, don’t gain weight and it’s an issue. I feel that the bigger issue isn’t how much or little is gained but the inner feelings around weight gain itself. Another paper published even discusses how weight stigma actually increases the chances of excessive weight gain, leading to higher rates of postpartum depression and weight retention.³ She wants communities and providers to focus more on how they’re treating pregnant people overall versus focusing on weight and all the factors that deals with.
And to turn it around a little bit, knowing how hard it is to be okay with weight gain in pregnancy and all that entails, I found an amazing post⁴ about some concrete ways you can feel a little more positive about your body during pregnancy. One of the big ones that I love to tell people is to get rid of the scale! You are not based on the number that shows up. You should be gaining weight, because your body is growing another human, expanding your blood volume, and creating a placenta, but weighing yourself regularly and at every appointment can be doing more harm than good to your mental health. And all this isn’t to say you won’t have bad days! “You’re going to have negative thoughts and feelings about your body sometimes so forget trying to be positive all the time. These thoughts are not a personal failure—we live in a culture that breeds body insecurity and bombards us with unrealistic beauty ideals daily.” One of their suggestions is to find positive sources instead, like the 4th Trimester Bodies Project.⁵
Just like any other time in your life, you are not defined by your weight. Pregnancy should be a time when you are eating well, growing healthy, building another human, not a time to focus on what the numbers mean or how our old clothes don’t fit anymore. Take it one day at a time and try to embrace the difference in your body. It’s not easy, but even small acts can help you feel better and have less depression and mental health issues than the focus on how your body is changing in a negative light.
Resources:
1. Breda, Joao. Body Image, Pregnancy, and Birth. http://www.euro.who.int/__data/assets/pdf_file/0003/277734/Body-image-and-pregnancy.pdf?ua=1
2. Bodnar, Lisa M. Prepregnancy Body Mass Index, Gestational Weight Gain, and the Likelihood of Major Depression During Pregnancy. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2760651/
3.Rodriguez, Angela C. Association of Weight Discrimination During Pregnancy and Postpartum with Maternal Postpartum Health. https://medicalxpress.com/news/2019-02-pregnant-women-weight-stigma-decreased.html https://www.ncbi.nlm.nih.gov/pubmed/30762402
4. Davidson, Megan. 7 Steps for a Body Positive Pregnancy. https://www.nationaleatingdisorders.org/blog/steps-for-body-positive-pregnancy
5. The 4th Trimester Bodies Project. https://www.4thtrimesterbodiesproject.com/
How Does Pregnancy After Loss Affect Perinatal Mental Health
Even though pregnancy loss is fairly common, especially in the first trimester, and is a physiological process, the grief and mental health ramifications can be life-long. If you have an early pregnancy loss before 12 weeks, many haven’t even told anyone they are pregnant and thus go through the release and grief process alone, compounding the mental health issues. So the question is, how exactly does pregnancy loss affect one’s mental health in the subsequent pregnancy?
Even though pregnancy loss is fairly common, especially in the first trimester, and is a physiological process, the grief and mental health ramifications can be life-long. If you have an early pregnancy loss before 12 weeks, many haven’t even told anyone they are pregnant and thus go through the release and grief process alone, compounding the mental health issues. So the question is, how exactly does pregnancy loss affect one’s mental health in the subsequent pregnancy?
The prevalence of PTSD one month after pregnancy loss was as high as 25%, with 34% of those with increased chances of depression. At four months, the rates of PTSD had fallen to 7%, but the rates of depression stayed the same, and the depression rates fell very slowly over the next few years.¹ In addition to this, a study done on anxiety and prenatal attachment in subsequent pregnancy after loss showed that those with a history of loss had greater risk of anxiety and less chance of prenatal attachment during pregnancy.² It’s been coined as “emotional cushioning”³, the emotional barrier you place between yourself and your unborn baby as if protecting yourself in case of another loss. The trauma and grief appear to be longreaching, affecting not only your mental state, but attachment to other children born after your loss.
To better understand how pregnancy loss affects the next pregnancy, I created an anonymous online survey with questions about their mental health in the next pregnancy, specific things that helped them, if they felt connected to that baby, if they felt capable of parenting that baby, and if their mental health got better or worse after the birth, among others.⁴ I received 84 responses in less than 3 days, all from online friends, their friends, and groups they shared the survey in. Of all the responses, all had had a pregnancy loss and either were currently pregnant again or had a pregnancy following that loss. 60% said that their grief from loss made their mental state worse during the pregnancy, mostly from fear of another loss, but it lessened after the live birth for 40% of those. One said, “I think I needed to fully grieve the babies I didn't carry full term in order to fully love the next baby that I did carry full term.” One question asked if they trusted their ability to parent the baby, 75% said yes, and a response in particular said, “Yes and no, I trust my ability as a parent but I also question myself more and have more anxiety.”
Two of the more intense questions dealt with thoughts of self-harm and suicide during their pregnancy after loss, and in both questions, around 11% had considered both. Because it’s anonymous and clumped together in the report, I don’t know if they were the same 10% of people, but it’s still a fairly high number to me. This shows me that pregnancy after loss isn’t just worry, fear, and emotional cushioning, it’s also a serious mental health concern that may make some people consider harming themselves along with suicide, and possibly act on it. As practitioners, whether doulas, midwives, or even just friends and family, we should be aware of this when working with or talking to those pregnant after loss.
Another interesting aspect of the survey showed that for more than 90% of those that responded, two things helped their fear and anxiety during pregnancy more than anything else: frequent ultrasounds and getting past the gestation of their previous loss. The fact that ultrasounds were the most common way for them to feel safe showed that they needed that outside validation of a growing baby that had more chance to survive through pregnancy and birth than the one before. Some were considered more high risk and under the care of Maternal Fetal Medicine Doctors, but even those with low risk pregnancies after a single loss still had the extra monitoring of their pregnancy just to keep their anxiety under control.
Pregnancy should be a time of excitement and joy, if the pregnancy is planned and wanted, and in many cases of pregnancy after loss the baby is not only planned but very much wanted. Perinatal mental health issues stemming from the loss make this time not a joyous and exciting one for many, and instead it’s a time filled with anxiety, depression, and emotional detachment. Considering one in four people have experienced a pregnancy loss, that is a lot of people going through a very probable mental health crisis during their next pregnancy, one where many don’t get the support they need because they feel guilt from the last loss, guilt to be pregnant again, or even shame that they don’t deserve this baby if they have untreated PTSD or severe anxiety or depression from their loss. We need to make sure we are aware of their history, the signs of anxiety and depression during pregnancy, and that we have the resources available to refer them for more help if they need it.
Resources:
Engelhard, Iris M. Posttraumatic Stress Disorder after Pregnancy Loss. https://www.sciencedirect.com/science/article/pii/S0163834301001244
Armstrong, Deborah. Pregnancy After Perinatal Loss, The Relationship Between Anxiety and Prenatal Attachment. https://onlinelibrary.wiley.com/doi/pdf/10.1111/j.1552-6909.1998.tb02609.x
Arsenault, Denise. Emotional Cushioning in Pregnancy After Perinatal Loss. https://www.tandfonline.com/doi/full/10.1080/02646838.2010.513115
Pearson, Kayce. Pregnancy After Loss Questionnaire Responses. https://docs.google.com/spreadsheets/d/1mMY5SNyuc7OyVlDo3s8Y8rzcj-rIzn3XSYPhEg_8a0w/edit?usp=sharing
Hemoglobin and Pregnancy
During pregnancy, hemoglobin is a touchy subject. In some cases, it is the only tool used to monitor iron levels and risk of anemia, but as stated above, hemoglobin is simply a screening marker.
Hemoglobin is the oxygen carrying component of red blood cells, and is a screening marker for problems, not a diagnostic tool. Your fingertip is pricked with a small lancet, a drop of blood taken and tested. All in all, it only takes a few minutes to know your hemoglobin status. It’s a valuable tool in any practice, but it isn’t the end all diagnostic for iron levels. Hemoglobin can also be checked in a blood draw lab test, included in the CBC, and those results can be more accurate than the quick finger prick.
During pregnancy, hemoglobin is a touchy subject. In some cases, it is the only tool used to monitor iron levels and risk of anemia, but as stated above, hemoglobin is simply a screening marker. One of the biggest changes to hemoglobin is a physiological decrease response to an increase in blood volume, which is normal in a healthy, well-nourished pregnancy. Falling hemoglobin levels and a well-growing baby coincide with each other, and they are an important factor in monitoring a healthy pregnancy.
Hemoglobin levels in pregnancy can be tested at any time, but generally are done at the first prenatal visit and then at the beginning of the third trimester, around 28 weeks. The first visit is a baseline value, normally done before 8 weeks of pregnancy, and shows what your hemoglobin is before your blood volume has expanded. Sometimes this first test can point to a lower than optimal beginning hemoglobin which can be corrected in most cases with diet and nutrition changes and supplements when needed.
In general, hemoglobin in the first trimester of pregnancy should be around 12-13g/dL, giving you enough room for a 2g fall by 28 weeks. At 28 weeks, Anne Frye says that the lower limit of normal is 10g/dL, but even then, hemoglobin is again just a screening marker.
During pregnancy, your hemoglobin will drop gradually as your blood volume increases, and you should see a 2g/dL drop by 28 weeks, IF you live in an area that is less than 5000 feet above sea level. Altitude matters in cases of hemoglobin levels! If you live between 5000 and 8000 feet, you may only see a drop of 1-1.5g/dL. If you are above 8000 feet, you may not see a drop at all. Your body has to compensate for the lower levels of oxygen in your area, and your hemoglobin will show that.
If your hemoglobin didn’t drop at all by 28 weeks and you live below 5000 feet, it’s a sign that your blood volume hasn’t expanded well, and can lead to problems with your baby’s growth and issues with blood loss and its effects after the birth.
Along this line, anemia is a marker of a problem, not a diagnosis, and hemoglobin alone is misleading as pregnancy advances. If your hemoglobin is low, or lower than where your provider would like, more tests are needed before any diagnosis is made.
LOW HEMOGLOBIN IS JUST A SCREENING MARKER.
If it’s low, the additional tests that may be run are serum iron, total iron binding capacity, transferrin saturation, and serum ferritin. In most cases, the serum ferritin may be the only additional test that is needed.
Ferritin is the major iron-storage protein, and the serum ferritin test is checking for available iron stores in bone marrow. This is more of an indicator of iron deficiency than hemoglobin. In normal menstruating women, the value should be 25-200ng/mL.
If your hemoglobin is low (again, below 10g/dL), serum ferritin should be the next test ordered to make sure your levels are within normal range. For most pregnant people, levels of ferritin below 30ng/mL confirms iron deficiency anemia. If this is run at the beginning of pregnancy, a hemoglobin level less than 11g/dL and serum ferritin level of less than 25ng/mL is the biggest sign that changes are necessary to increase both levels. In some cases, that can also point to other issues with iron and red blood cells, but that is more rare than simply being iron deficient.
Remember: Normal hemoglobin levels after 28 weeks of pregnancy are above 10g/dL, but it is simply a screening tool. More testing is needed, specifically a serum ferritin, which should be between 30-200ng/mL, showing that you are not anemic, your risk of bleeding during birth is not increased, and your hemoglobin level is not an issue.
RESOURCES:
Understanding Diagnostic Tests in Childbearing Year by Anne Frye, pages 258-298, Normal Hemodilution, Anemia, and Red Cell Disorders in Pregnancy.
Holistic Midwifery Vol 1 by Anne Frye, pages 195, 580, 828-832, 1007-1008.
https://www.uptodate.com/contents/maternal-adaptations-to-pregnancy-hematologic-changes/abstract/5" target="_blank">Hematological Changes
https://www.ncbi.nlm.nih.gov/pubmed/19935037" target="_blank">Pregnancy and Laboratory Studies
Experience Doesn't Pay the Bills!
Unpaid internships are almost a staple in the United States, a thing of privilege, and in my opinion, a thing that needs to be dismantled. I’m not saying it will happen overnight, but I think steps need to be taken to get rid of this archaic system, propped up by privilege and tradition.
I’ve been a birthworker for ten years, from doula to midwifery assistant to midwife myself, and one thing I’ve seen over and over is the idea that experience is a currency we can use to avoid paying actual money to those that help us.
Unpaid internships are almost a staple in the United States, a thing of privilege, and in my opinion, a thing that needs to be dismantled. I’m not saying it will happen overnight, but I think steps need to be taken to get rid of this archaic system, propped up by privilege and tradition.
“I had to do my apprenticeship for free (or even had to pay for it), and it made me learn better/faster/what have you, and I think we should continue it.”
How many times as a birthworker have you heard that? Did it make you more excited to get into the field, or did it seem like an impossible barrier so your dream would never come to fruition?
Being on call for weeks at a time has its own set of challenges, and doing it for free makes it even more challenging. Most birthworkers have children that need care while you’re away, a working car with a full gas tank, and some apprenticeships even require you to have certain equipment before you can begin or to pay a fee to attend the birth, and if you are working for free, your partner needs to be working a great job to cover your expenses, or you need to have another source of income while doing this work while also having the freedom to be on call and leave whenever you need. All of this can lead to burnout, additional stress and worries, and for a lot of people, the inability to even be able to do an apprenticeship which would line up in every other way except for finances.
If we are requiring certain trainings, tools, resources, and more as a minimum for people to even consider working for and with us, why are we letting an antiquated system decide how we can support them in their process? Why are we content with putting our past experiences in the forefront, saying that nothing can change because we didn’t have the option of not only payment, but more things on top of that?
In a world that is ever changing, why are we so content in the idea that experience is equivalent to cash?
It’s not a new idea. Artists, freelancers, and many more careers off the beaten path have been told for years that exposure = payment, and it’s just not true. Why is it that interns in a hospital are paid (though it is bare minimum), but apprentices for a midwifery practice are told to find another way to make it work because the experience is the payment? In what world is experience a currency that can not only pay bills and keep a roof over your head, but make you want to truly be in that field and not feel like someone just there as unpaid labor?
Our world requires money to live. I wish it wasn’t that way. Insurance is expensive, cars are expensive, housing is expensive, food is expensive. Experience doesn’t pay for any of that.
When I did my apprenticeship, I was privileged to have a supportive partner and supportive friends. I didn’t have to worry about what to do with my child if I was called to a birth, which was a massive load off my mind. I didn’t have to worry about filling the tank to get to a birth because we had a bit of money to spare to make sure I could.
And yet, I can’t help thinking about what it would have been like to not put all that pressure on my partner and our relationship. What would it have been like if I had been able to provide at least a little bit back to help buy food, to buy gas, to pay for our car insurance. I would have been more willing to be a part of the experience, I would have eagerly joined in on more events. Being paid would have given me a buffer, an ability to breathe a little should something outside our very tight budget happen.
What if we decided to change this paradigm and tradition. What if instead of saying “Well I had to….” we instead said, “I did mine for free, but you don’t have to.” What if instead of putting the responsibility outside ourselves, watching person after person quit, leave, or burnout, we gave them a little bit of financial security in exchange for their presence, training, and help. Even if the relationship doesn’t last as long as we want, or they decide to pursue another path, what if we put the effort in and showed our appreciation with a little bit of monetary compensation for the work they do so we can focus elsewhere.
We don’t need to perpetuate a harmful tradition anymore.
Just think of how many more birthworkers we could create if we simply said, “No more.”
Open, Open, Open
I wrote this last year, a poem about the last fifteen or so minutes of my last labor and birth. It was the longest and shortest six hours of my life, and time had no meaning until it did. Everything was quiet, and I loved it. I worked with my body, I moved, I moaned, I spoke, I whispered.
I wrote this last year, a poem about the last fifteen or so minutes of my last labor and birth. It was the longest and shortest six hours of my life, and time had no meaning until it did. Everything was quiet, and I loved it. I worked with my body, I moved, I moaned, I spoke, I whispered.
In the end, it was the most amazing experience of my life.
"Open, Open, Open"
Kayce Pearson
“Open…open…open…”
I chant to myself as I float in the pool.
Silence aside from me.
My family sleeps in the other room
My friend rests on the couch, keeping vigil.
I turn inward, willing my body to relax;
Another contraction.
I lift my body, floating on my back.
“Open…open…open…”
Peak. Tears well.
Can I do this?
I float back down to rest.
Time has no meaning; I float.
I smell steam.
The water engulfs me.
My body is no concern.
Just the sensations; the air, the water.
My phone rings, its sound jars me from my mind.
ANGRY! Disjointed.
How can it be 7:15?
Why aren’t you born??? I growl.
Did I say it aloud?
No. No. I can’t.
Another contraction; this time so long to focus.
“Open…open………”
It feels different.
My pelvis moves.
I gasp.
I feel it, a head rotating
Moving down
I know then the work is beginning.
I flip over onto my knees,
I lean over the edge of the pool.
Focused.
“Get Blake!” I yell. I regret it.
No time. Work to do.
I feel my uterus push. I growl and help it. Yes.
The air feels heavy.
Everyone runs out. Blake wraps his arms around me;
He whispers to me.
I tune it out. I just needed his strength.
Another push.
“I see a head!”
Head is out.
I push. My uterus pushes.
Nothing.
Anger. Why won’t you move?!
I feel a body inside me rotate.
No logical thought.
All that matters is the feeling.
Is he stuck?
Push. Turns. Growls. Push.
Release.
All emotions cease.
The room is silent.
Breath is held.
I turn over, grab my baby.
I pull him to the surface of the water,
“It’s a boy!” I yell.
Noise all around. “You did it!”
I sit higher.
“Come on baby. Breathe for mommy.”
He wiggles. No breath.
I talk to him. I rub him.
I love him.
I am calm.
Then.
A cry.
Close to the Bones Podcast Episode #3
In which I talk about the energy of transition, the time between water and air, and wonder why we’ve come so far from understanding that some things we will never understand.